W-Sitting: Things to Consider
Hello! My name is Hannah Nielsen and I am an occupational therapist (OT)at Partners In Excellence. I have been practicing as an occupational therapist for just over 2years and treat clients at our North St. Paul location. One of the many reasons that I love Partners is that I can promote independence across a variety of skills while working as part of a collaborative team. I am currently supervising a level II fieldwork student, Chrissy Vang, who also participated in writing this blog post.
Today we will be discussing W-Sitting.
What is W-Sitting?
W-sitting occurs when someone is sitting flat on the floor with their knees turned inward and feet pointing out. When observing this posture while standing, it visibly forms a “W”. This sitting position is often observed during childhood, but it may naturally decrease as the child matures.
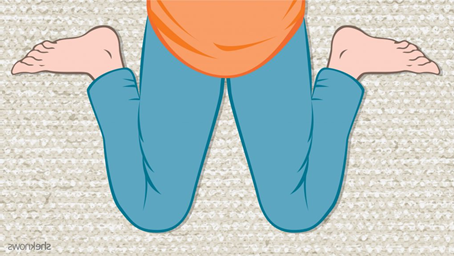
(Autism Alliance, 2019)
Potential Reasons This Occurs
- Poor core strength
- When a child has insufficient core strength or poor posture, a “W” sit provides a wider base of support which requires less engagement from core and trunk muscles. Children with low muscle tone may utilize a “W” sitting position as a compensatory strategy to preserve energy.
- Sensory seeking – Proprioceptive input
- Proprioceptive input is the ability to feel where your body is in space. When a child engages in seeking out proprioceptive input, they may not be able to sense their body’s movements or corresponding actions. During pretend play, a child may automatically bring a toy phone to their ear without overshooting. Or when a child is thirsty, they can bring a full cup of water to their mouth to drink without spilling. These examples demonstrate a sensory system that is functioning properly to help a child perform a desired action by recognizing where their body is in space.
- Repetitive positioning
- A child may position their body into a “W” sit as it provides a more comfortable sitting posture. Out of routine or habit, they may naturally position themselves into this posture without realizing it.
How Does OT Address W-Sitting?
- Strengthening
- OTs can help the individual strengthen specific muscle groups to improve sitting balance and postural control. This could either be in the form of an individualized exercise program or during playful therapeutic activities and engagement.
- Positioning
- An OT may provide visual supports or alternative positioning for a child to help correct a “W” sit.
- An example of a visual support that includes alternative positioning is included below:
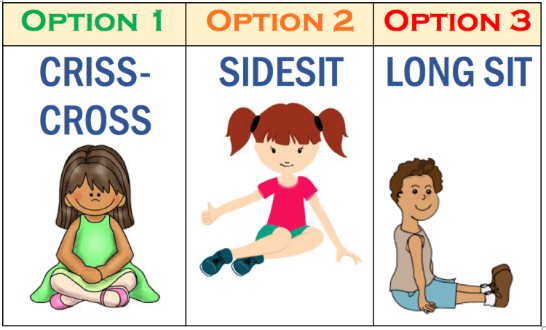
(Autism Alliance, 2019)
- Balance
- A child may participate in different balancing activities with their OT to improve their body awareness and postural control. This will help to improve a child’s sitting and standing balance across environments.
- Coordination
- OTs may include a variety of activities such as crossing over from one side of the body to the other (crossing midline) and using both the upper and lower body to complete tasks (bilateral coordination). By increasing a child’s coordination, they will have a greater range of motion and more controlled movements to engage in functional activities throughout the day.
Things to Try at Home
- Kid friendly yoga
- Visual supports
- Proprioceptive sensory input
- Exercising
- Gross motor play activities
- Some examples could include:
- Jumping jacks, hopscotch, crab walks, bear crawls, etc.
- Some examples could include:
For more information or concerns you have may, please consult with your occupational therapist.
Our occupational therapy team is excited to continue to contribute to our Partners’ blog this year to offer insight into our field. Be on the lookout for more posts from our occupational therapists and certified occupational therapy assistants!
References
Autism Alliance. (2019, May 23). W Sitting. http://www.autismalliance.com.au/w-sitting/


Recent Comments